(January 28, 2023) The fundus camera, an instrument used in opthalmology for to capture colour images of the inner surface of the eye, can set one back by anywhere between INR 1.5 lakh and INR 5.25 lakh. In low-income countries, the prohibitive cost of devices used in diagnostic and rehabilitative care makes access a challenge. According to the World Vision Report, prepared by WHO, over 2.2 billion people worldwide are visually impaired and nearly half that number live with treatable or preventable conditions because they cannot get the care they need. The second-leading cause of blindness is glaucoma, with an estimated 57.5 million people around the world affected by primary open-angle glaucoma. In 2020, according to the National Center for Biotechnology Information, this number rose to 76 million. Among those tackling the problem head-on is Ontario teen Hardit Singh whose innovation is a step towards better healthcare for all.
Speculor: A Comprehensive Teleopthalmology Platform for People Centered Eyecare fetched seventeen-year-old Hardit the top prize at the Canada-Wide Science Fair in 2021. Using a portable imager and AI algorithms to screen for disease, Speculor, which has been field-tested in India, can detect glaucoma for the very-affordable sum of $300. The Global Indian, who also won second place at the European Union Contest for Young Scientists, intends for the device to be used by international NGOs working to bring equality in eyecare.
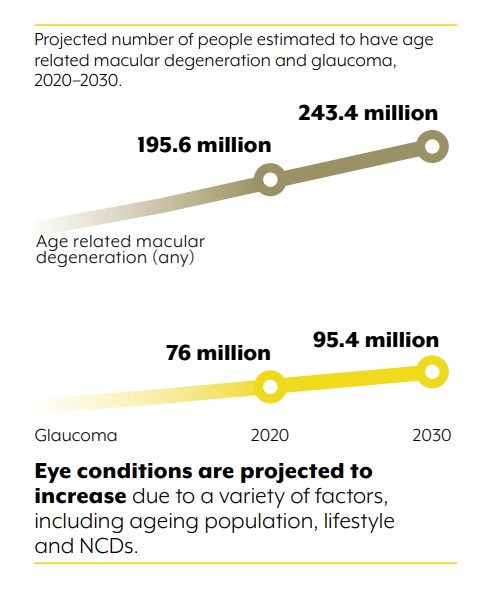
Source: World Vision Report
The vision
Born and raised in Waterloo, the idea took root around three years ago, when a friend from the Cameron Heights Collegiate in Kitchener, where Hardik studied, suffered from retinal detachment, where the retina begins to peel off the eye. “He went to three different opthalmologists and experts and was misdiagnosed all three times for different reasons. He went almost blind because of it,” Hardit said in an interview for the Canada-Wide Science Fair. Luckily, doctors managed to detect it before the damage became irreversible. It made Hardit wonder – if such misdiagnoses can happen in a place like Waterloo, what could conditions possibly be in rural or low-income areas, where there is little proximity to healthcare facilities?
By this time, the then 13-year-old Hardit was already building classification algorithms and had a basic understanding of AI from previous projects. He hit the books, learning from YouTube, books and just “trying things out, playing around until it works. That works for hardware, you tinker until you understand what happens. It’s the same with optics. I learned until I had enough to build what I wanted.”
He began cold-emailing professors, eventually hearing back from the University of Waterloo’s Department of Optometry. Hardit began working with a group of grad students, going to them with questions or when he was struggling. The hardware had to be built, the software coded and the two integrated. He worked in the lab, testing the device on a model eye in controlled conditions.


Hardit Singh
Challenges and stepping stones
Speculor worked smoothly in the lab and Hardit decided to roll out his prototype. When he tested it on the field, however, “everything failed,” he admits. He had made one fundamental mistake – he hadn’t geared the device for less than optimal conditions. “I had designed the prototype to work in perfect condtions but in poor lighting, when the patient is moving around, the device wsn’t working at all. The AI had the same problem.” The AI sensor was used to very high-quality images, taken by devices, Hardit says, that cost USD 25,000 and up. “My device can’t produce such images and it was throwing the AI off.”
“I was frustrated. I had put in so much effort and the device didn’t work at all. But my mind was already working on how to fix it.” With the hardware, his moment of revelation came through integrating cross-polarisation, a technique used in more expensive fundus cameras but rarely in more affordable devices. “It worked really well to ensure there was no glare on the fundus images,” he said. He tried a number of solutions with the AI, but nothing worked, until he developed his own training method. The AI was trained to study low quality images, account for poor lighting and movement and detect anomalies under these parameters.
Hardit Singh sent the device for testing once more, this time to an opthalmologist in India. The feedback was far more promising. “The second time, the images turned out really good. It was amazing because I still wasn’t expecting it to work, I only had acess to a model eye. This was a Hail mary move for me, sending a protype to India blindly without a test.”


Source: The Record
Always a work-in-progress
Hardit’s eventual goal is to commercialise the device, pricing it within reach of international NGOs and organisations, to improve healthcare in rural and underserved areas around the world. The cost is currently dominated by the lens, which is about $250. He is also working to improve the design, after a judge from the CWSF remarked that it was “too boxy.”
Hardit Singh also wants to expand the scope of his device, which is now mainly used in glaucoma detetion. “I can reapply the same model over different diseases by changing the paramters,” he says. He also wants to make it easy to understand, to aid doctors as they make a diagnosis.
Hardit has also published a paper on AI in the Journal of the Optical Society of India. His other interests include computer science, AI, optics, medicine and sports.



